Host adaptation strategies of avian influenza A viruses for better replication in human - State Key Laboratory for Emerging Infectious Diseases and the Department of Microbiology, Li Ka Shing Faculty of Medicine, the University of Hong Kong
20 Nov 2014
Host barriers block cross species transmission and replication of animal viruses in humans. Such host restriction mechanism limits the transmissibility and the ability of the avian virus to cause mammal and human infections. However, research team led by Dr. Honglin Chen, Associate Professor, and Professor Kwok-yung Yuen, Henry Fok Professor in Infectious Diseases, Chair Professor of Infectious Diseases from the Department of Microbiology, Li Ka Shing Faculty of Medicine, and State Key Laboratory for Emerging Infectious Diseases, the University of Hong Kong, found that avian influenza viruses may gain the ability to replicate in mammal and human cells through various adaptation changes in one of the viral replication complex subunits called the PB2, causing infections and diseases in humans. The discovery has been published recently in Nature Communications, in which team members Drs. Wenjun Song and Pui Wang are co-first authors.
Background of the study
Multiple avian influenza viruses have caused human infections in many countries since 1997. Among these cross human infections, avian H5N1 virus has since caused more than 600 human infections with over 50% of them are fatal; while avian H9N2 virus causes only relatively mild diseases, serological and receptor studies showed this virus has certain degree of ability to infect humans; the emergence of a novel H7N9 virus in East China since 2013 has led to over 400 human cases with 30% of those infections being fatal; apart from H5N1, H9N2 and H7N9 avian influenza A viruses, human infections with H10N8, H6N1 and H5N6 subtypes of avian influenza were also reported in China and Taiwan respectively in recent years. Understanding the molecular basis for the cross species transmission is the key in the preparedness for the future pandemic which is deem to happen but we could not predict the time and the subtype of virus which may emerge.
Binding to cell receptor through the hemagglutinin (HA) of virus is the first step in initiating infection. Current knowledge showed that the HA from most of the avian influenza A viruses have certain levels of ability to bind to human respiratory tract cells. However, only a limited number of avian influenza A subtypes have caused human infections. What are the other viral elements which determine the ability of avian influenza A viruses to cause cross species transmissions besides receptor binding? Why some avian influenza A viruses appear more likely to cause human infections? Are we able to monitor changes in avian influenza A virus to predict the likelihood of cross human infections? All these are questions that we need to answer for our preparedness of potential future pandemics. Because of the host barriers, avian influenza A virus may not be able to replicate when it gets into human cells. The host barrier is the host restriction of virus replication. Nevertheless, virus may undergo adaptive mutation to gain the ability to replication in human cells and cause diseases in humans.
Research findings
In a recent study reported in the Nature Communications, a research team led by Dr. Honglin Chen, Associate Professor, and Professor Kwok-yung Yuen, Henry Fok Professor in Infectious Diseases, Chair Professor of Infectious Diseases from the Department of Microbiology, Li Ka Shing Faculty of Medicine, and State Key Laboratory for Emerging Infectious Diseases, the University of Hong Kong, found that avian influenza A H5N1 and H7N9, and seasonal H3N2 viruses may gain the ability to replicate in mammal and human cells through various adaptation changes in the viral replication enzyme complex called the PB2 subunit. They found that H7N9 avian influenza A virus is able to utilize multiple adaptive strategies to replicate in human cells, which may explain why H7N9 is distinct in causing human infections; This study identified a novel adaption marker, PB2-526R among some H7N9 viruses and almost exclusively among all H5N1 human cases from Indonesia. It has been a puzzle why there is no known PB2 adaptation marker in the H5N1 virus from Indonesia human cases and the finding from HKU nicely explained how this Indonesian subclade of avian H5N1 virus may have adapted for human infections. This study also found PB2-526R is able to enhance replication and pathogenicity of other types of PB2 adaptations, such as previously known PB2-627K, in H7N9 and H3N2 viruses. Since the human pandemic H3N2 virus emerged in 1968, it has gained an additional PB2-526R adaptation marker since 1970s and the PB2-526R-627K virus replicates better than the solely PB2-627K virus. It is likely that the impression of more severe disease burden caused by H3N2 than that of H1N1 may be partly attributed to the better replication ability of PB2-526R-627K virus. These findings by HKU provided new insight for the understanding of cross species transmission and replication in human cells by avian influenza viruses. The study provides a new genetic marker for the surveillance of avian influenza A virus with potential for human infection.
To use the press release photo(s) for any publishing, publicity and related purpose, photo courtesy should be given to “Li Ka Shing Faculty of Medicine, The University of Hong Kong”
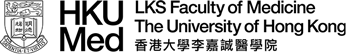
Cells infected by avian influenza A viruses without PB2 adaptation marker.
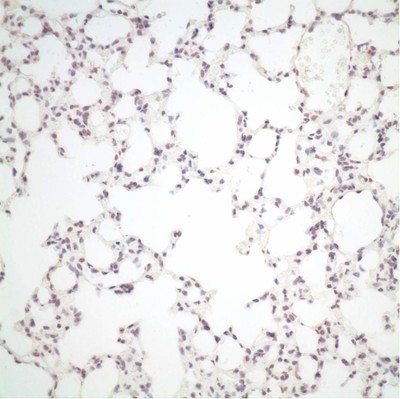
Cells infected by avian influenza A viruses with PB2 adaptation marker, cells in brown colour are cells replicated by infection.
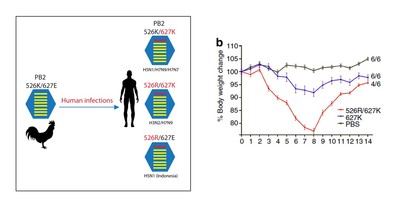
Replication adaptation of Avian influenza A virus in humans.