26 February 2024
A research team from the LKS Faculty of Medicine at the University of Hong Kong (HKUMed) has successfully developed a neutralising monoclonal antibody, 6H2, which targets a harmful protein known to exacerbate damage caused by ischaemic stroke. Through pre-clinical experiments on animals, the team found that the 6H2 antibody effectively attenuates ischaemic stroke injury, offering potential for a highly effective pharmacological therapy for patients with ischemia stroke.
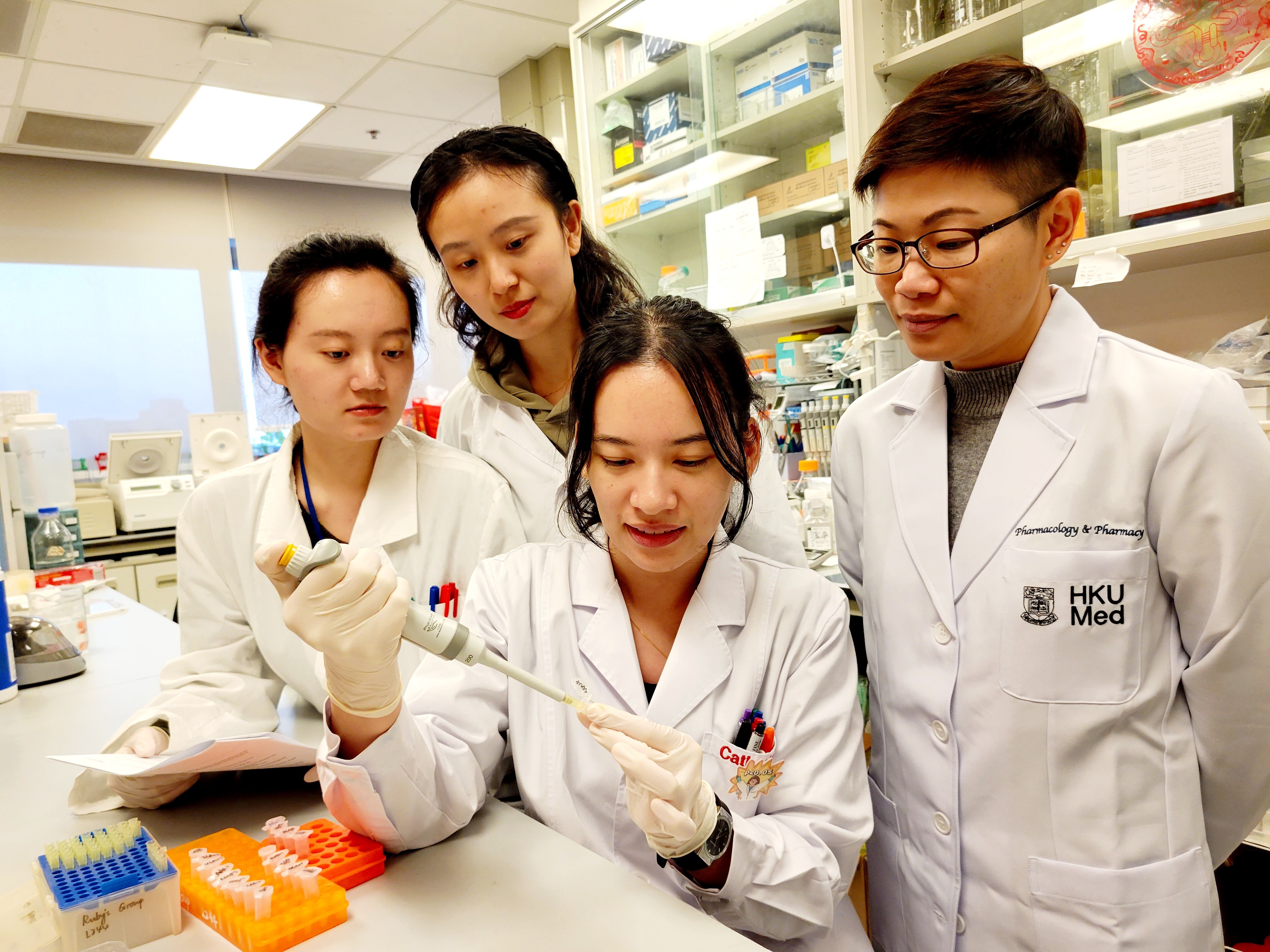
This remarkable breakthrough is the result of the concerted efforts of research teams from HKUMed's Department of Pharmacology and Pharmacy, the State Key Laboratory of Pharmaceutical Biotechnology, and the Department of Medicine, School of Clinical Medicine, HKUMed, as well as the Shenzhen Institute of Advanced Technology, Chinese Academy of Sciences. The findings were published in the Journal of British Pharmacology [link to the publication], and patent applications for the newly developed 6H2 antibody were filed in China, Europe and the United States.
Background
Stroke is a major cause of permanent disability and death worldwide. In Hong Kong, 13,500–14,000 individuals suffer from stroke every year, 80% of whom are diagnosed with ischaemic stroke, caused by blocked brain blood vessels. Currently, there are limited treatment options; tissue plasminogen activator (tPA) is the sole FDA-approved drug. However, tPA has potential side effects, like brain bleeding, and must be administered promptly. Novel therapies are therefore urgently needed.
The harmful protein that worsens ischaemic stroke is adipocyte fatty acid binding protein (A-FABP). HKUMed researchers discovered that A-FABP disrupts the blood-brain barrier by inducing matrix metalloproteinase 9 (MMP-9), worsening the effects of stroke. Higher circulating A-FABP levels were observed in mice with middle cerebral artery occlusion (MCAO) surgery and stroke patients, implicating it as a potential therapeutic target. A previous study of the HKUMed research team found that an A-FABP inhibitor, BMS309403, showed promise but other studies demonstrated potential side effects on the heart. Therefore, a specific and potent monoclonal antibody to neutralise the protein may be a better therapeutic strategy for ischaemic stroke.
Research method and findings
The researchers evaluated the impact of circulating A-FABP in ischaemic stroke by conducting experiments on A-FABP-deficient mice. The mice were replenished with synthetic A-FABP (rA-FABP) into the bloodstream and were then subjected to MCAO surgery to simulate a stroke. The replenishment of rA-FABP worsened stroke outcomes, resulting in larger infarct size, brain swelling, more severe neurological deficits, and a lower survival rate. These findings highlight the detrimental effect of circulating A-FABP in ischaemic stroke outcome.
Using the mouse hybridoma technique, the research team generated monoclonal antibodies targeting A-FABP. The monoclonal antibody 6H2 demonstrated strong binding to A-FABP in both humans and mice. 6H2 can effectively block harmful A-FABP effects, including certain protein activation and MMP-9 production in macrophages, which can cause inflammation and damage. The efficacy and safety of 6H2 were further evaluated in both mice with simulated strokes and healthy mice.
In wild-type mice with MCAO surgery, 6H2 treatment significant alleviated blood-brain barrier disruption, reduced brain swelling, decreased infarction size, improved neurological function, and lowered mortality risk. These positive effects were observed by a reduction in cytokines and MMP-9 production, known contributors to inflammation and tissue damage. Long-term 6H2 treatment had no obvious adverse effects in healthy mice, confirming its safety. These findings establish circulating A-FABP as a promising target for ischaemic stroke treatment, validating 6H2 as a potential monoclonal antibody drug candidate.
Significance of the study
Based on these groundbreaking findings, ‘our team is now collaborating with the Shenzhen Institute of Advanced Technology, Chinese Academy of Sciences to identify the structural determinant of 6H2 action and advance its humanisation,’ said Professor Ruby Hoo Lai-chong, Assistant Professor, Department of Pharmacology and Pharmacy, HKUMed.
‘With the pre-clinical evaluation of the humanised neutralising monoclonal antibody on the horizon, we are optimistic that these efforts will lay the foundation for a revolutionary approach to the treatment of ischaemic stroke,’ added Professor Hoo.
About the research team
The research was led by Professor Ruby Hoo Lai-chong, Assistant Professor in the Department of Pharmacology and Pharmacy, HKUMed, and Co-investigator in the State Key Laboratory of Pharmaceutical Biotechnology, HKU; and Professor Chang Junlei, in the Shenzhen Institute of Advanced Technology, Chinese Academy of Sciences. The co-first authors are Dr Liao Boya, post-doctoral fellow in the Department of Pharmacology and Pharmacy, HKUMed; and Dr Yang Shilun, Research Assistant Professor in the Shenzhen Institute of Advanced Technology, Chinese Academy of Sciences.
Acknowledgements
This study was supported by the Science, Technology and Innovation Commission of Shenzhen Municipality, the Innovation and Technology Fund, the Guangdong-Hong Kong Technology Cooperation Funding Scheme, the Area of Excellence Scheme of the Research Grants Council, the National Natural Science Foundation of China, the CAS-Croucher Funding Scheme for Joint Laboratories, the International Collaboration Project of the Chinese Academy of Sciences, and the Guangdong Innovation Platform of Translational Research for Cerebrovascular Diseases.
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email (medmedia@hku.hk).
Follow HKUMed