02 October 2024
A research team from the Department of Orthopaedics and Traumatology, School of Clinical Medicine, LKS Faculty of Medicine at the University of Hong Kong (HKUMed), has conducted the largest clinical trial on brace weaning to date. The study revealed that immediate brace removal is the preferred strategy for patients with adolescent idiopathic scoliosis (AIS) once their skeletal development is mature, providing effective evidence to cancel the current standard protection period. The team discovered that gradual weaning, with night-time brace wear for an additional six months, offers no advantages in maintaining spinal curvature or enhancing the patients' health-related quality of life (HRQoL). This pivotal finding could reshape treatment protocols for AIS, prioritising patient well-being over the uncertain benefits of prolonged brace use. The findings of the clinical trial were published in the journal JAMA Pediatrics [link to publication].
Background
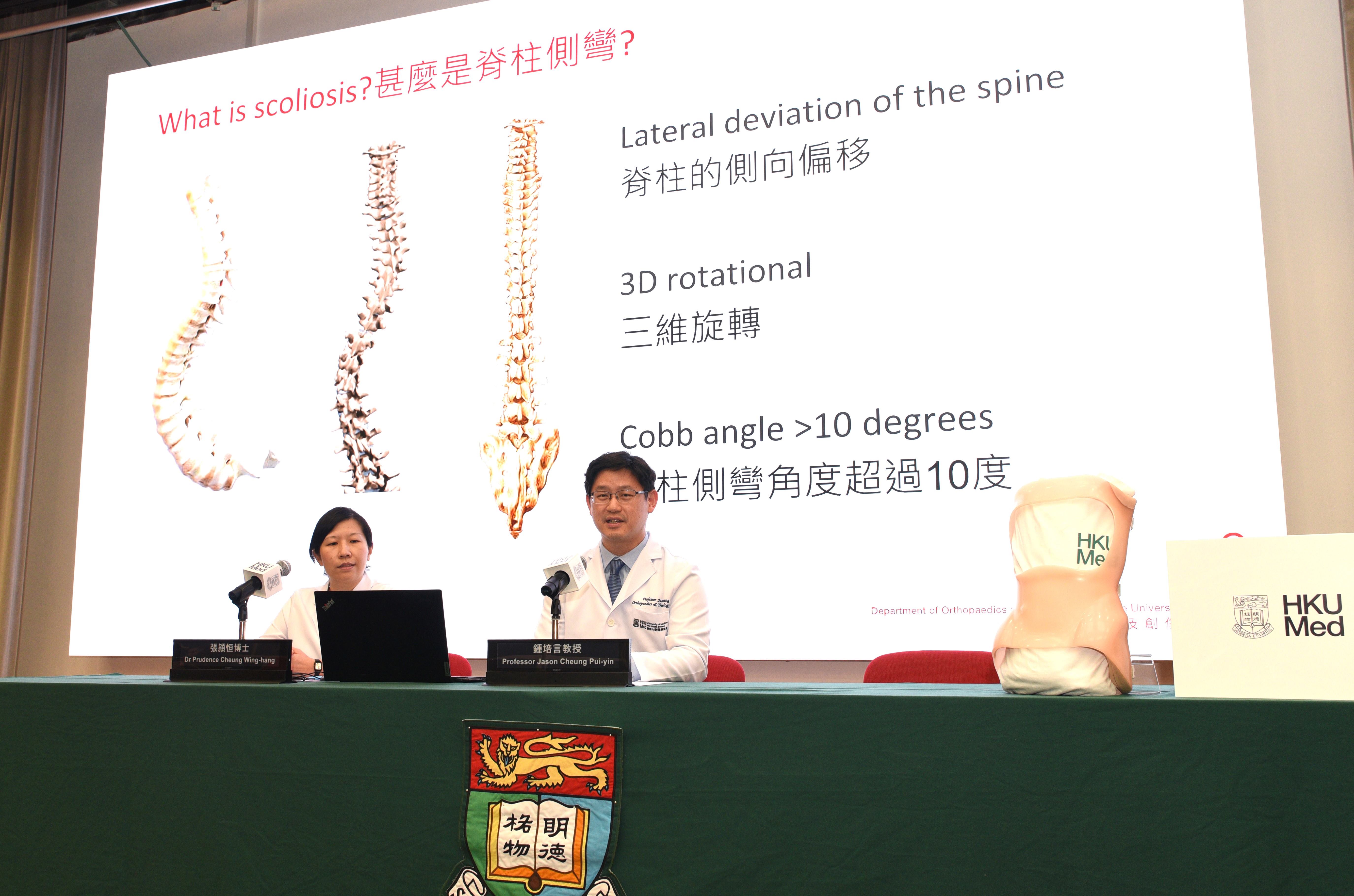
Idiopathic scoliosis is a lateral spinal curvature, whose cause is unknown, affecting 3–4% of adolescents in Hong Kong. It is more common in females (8:2 ratio). According to the standard criteria from the Scoliosis Research Society, bracing is recommended for skeletally immature patients with spinal curves between 25 and 40 degrees, particularly for girls who are pre-menarche or within one year of menarche onset and have not received prior treatment.
The aim of bracing is to prevent worsening curvature during rapid growth phases, especially during puberty, to avoid the need for surgery. Orthopaedic specialists prescribe braces that are custom-made for optimal comfort. Currently, there is a lack of evidence and consensus regarding the brace-weaning protocol for AIS. Many clinicians recommend gradual weaning to prevent curve deterioration after removal, which can lead to prolonged brace wearing and negatively affect spinal stiffness and HRQoL.
Research method and findings
From 2017 to 2020, the research team recruited 369 patients with AIS who had undergone underarm brace treatment and reached skeletal maturity at the Duchess of Kent Children's Hospital. A randomised controlled trial was conducted over the following two years, from 2020 to 2022, along with follow-up studies. According to the pre-set randomisation sequence, 193 patients were allocated to the immediate brace-removal group, and 176 patients followed a gradual weaning protocol, which entailed an additional six months of night-time wear before complete cessation.
The research team investigated changes in major curve size and truncal balance of the patients through routine spine radiographs and patient questionnaires at follow-up intervals of 6, 12 and 24 months. They also assessed HRQoL using refined Scoliosis Research Society 22-item (SRS-22r) and EuroQol five-dimension questionnaires. The findings indicated minimal differences of changes between the two groups, with a mean difference of less than one degree for the major curve and 1.5 degrees for minor curve in terms of curve size, truncal balance and HRQoL.
Further analysis revealed that skeletal maturity and major curve Cobb angle at the time of weaning were the key factors influencing curve progression two years after brace treatment, and the weaning protocols showed no correlation with curve deterioration after brace treatment. The team also compared the changes in truncal balance between the two groups, which revealed that both immediate and gradual weaning effectively maintained comparable truncal balance. Key parameters assessed included truncal shift, listing, shoulder height, thoracic kyphosis and lumbar lordosis. These are the crucial indicators of how well the patients balance their torso with the presence of the spinal curve.
Importantly for patient care, the research team also found that the patients' HRQoL was similar for both weaning protocols. Conventionally, gradual weaning is considered a better way to help alleviate muscle discomfort that can arise from sudden strain when transitioning away from the brace, as immediate weaning is believed to lead to more back pain. However, both weaning protocols demonstrated comparable HRQoL outcomes, including overall quality of life and specific aspects, like pain. The SRS-22r pain domain scores showed no significant differences between the two groups at any follow-up time-point, and the EQ-5D scores further confirmed that overall quality of life was similar for both weaning strategies.
Significance of the study
There is a lack of evidence and consensus regarding brace-weaning protocols for AIS worldwide, often leading clinicians to prescribe gradual weaning even when patients have reached skeletal maturity. This prolonged bracing can lead to muscle weakness, spinal stiffness and continuous discomfort associated with brace wear.
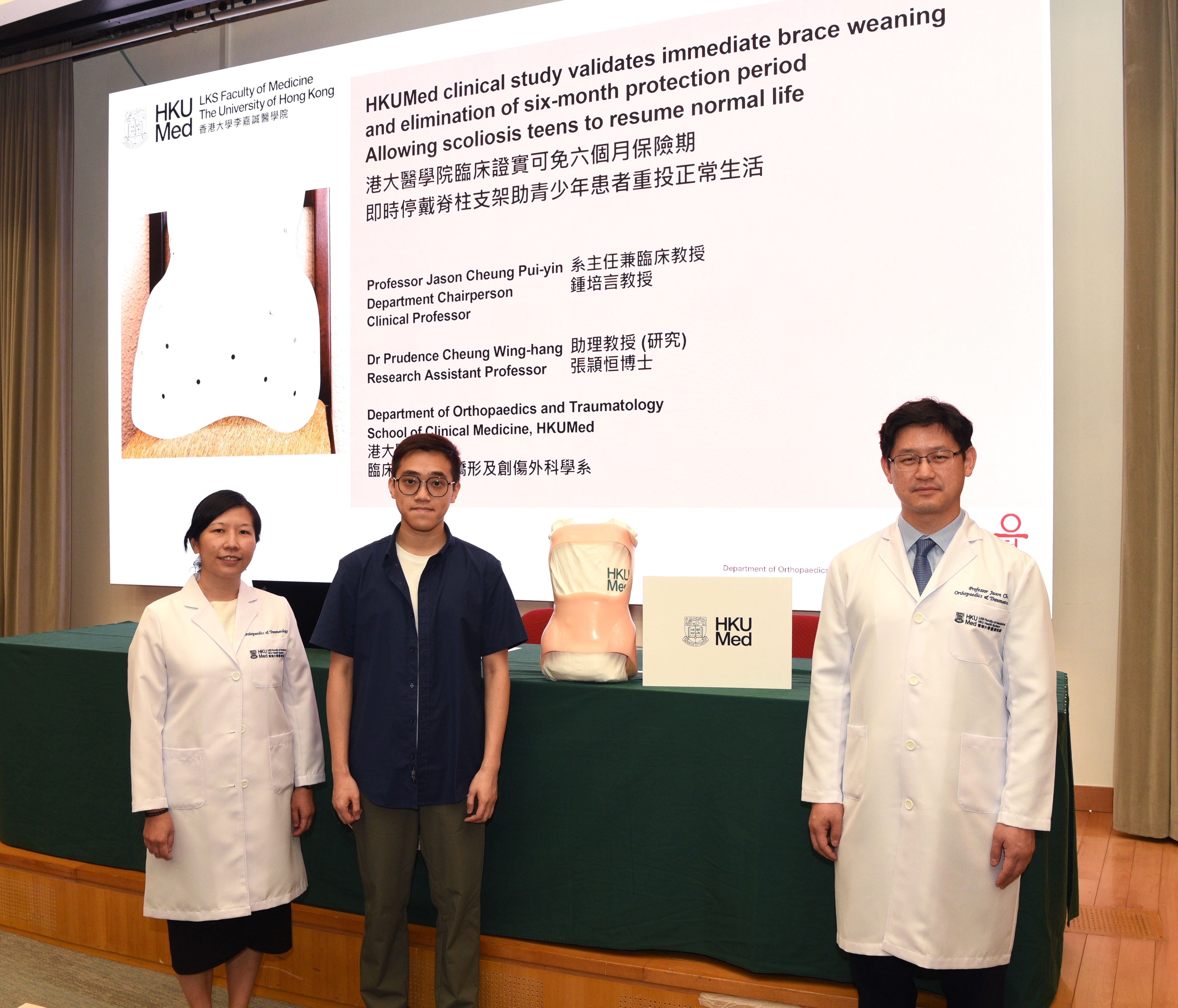
‘This largest randomised controlled trial on AIS brace weaning across the globe provides compelling evidence that gradual weaning is not superior to immediate weaning, as was commonly believed. Appropriate cases should now be considered for immediate weaning, which allows patients to return to higher levels of physical activity and exercise earlier. The approach will help avoid the overuse of brace treatment and facilitate a quicker return to normal life, helping them regain their confidence,’ said Professor Jason Cheung Pui-yin, Chairperson and Clinical Professor in the Department of Orthopaedics and Traumatology, School of Clinical Medicine, HKUMed.
This clinical trial provides high-quality evidence that could significantly impact clinical practice in the future. ‘We deeply appreciate the commitment of the research team, as well as the efforts and contributions of all participating patients and their families,’ commented Dr Prudence Cheung Wing-hang, Research Assistant Professor in the same department. ‘HRQoL is a crucial aspect that our spine surgeons consider, in addition to the scoliotic curves presented by patients. Through the use of specific questionnaires and expertise analyses, we elicit patients' HRQoL and enable our clinicians to effectively gauge their overall well-being during and after treatment.’
About the research team
The research was led by Professor Jason Cheung Pui-yin, Chairperson and Clinical Professor; and Dr Prudence Cheung Wing-hang, Research Assistant Professor; both from the Department of Orthopaedics and Traumatology, School of Clinical Medicine, HKUMed.
Acknowledgements
This research was supported by the Hong Kong Government's Health and Medical Research Fund
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email (medmedia@hku.hk).
Follow HKUMed