11 July 2024
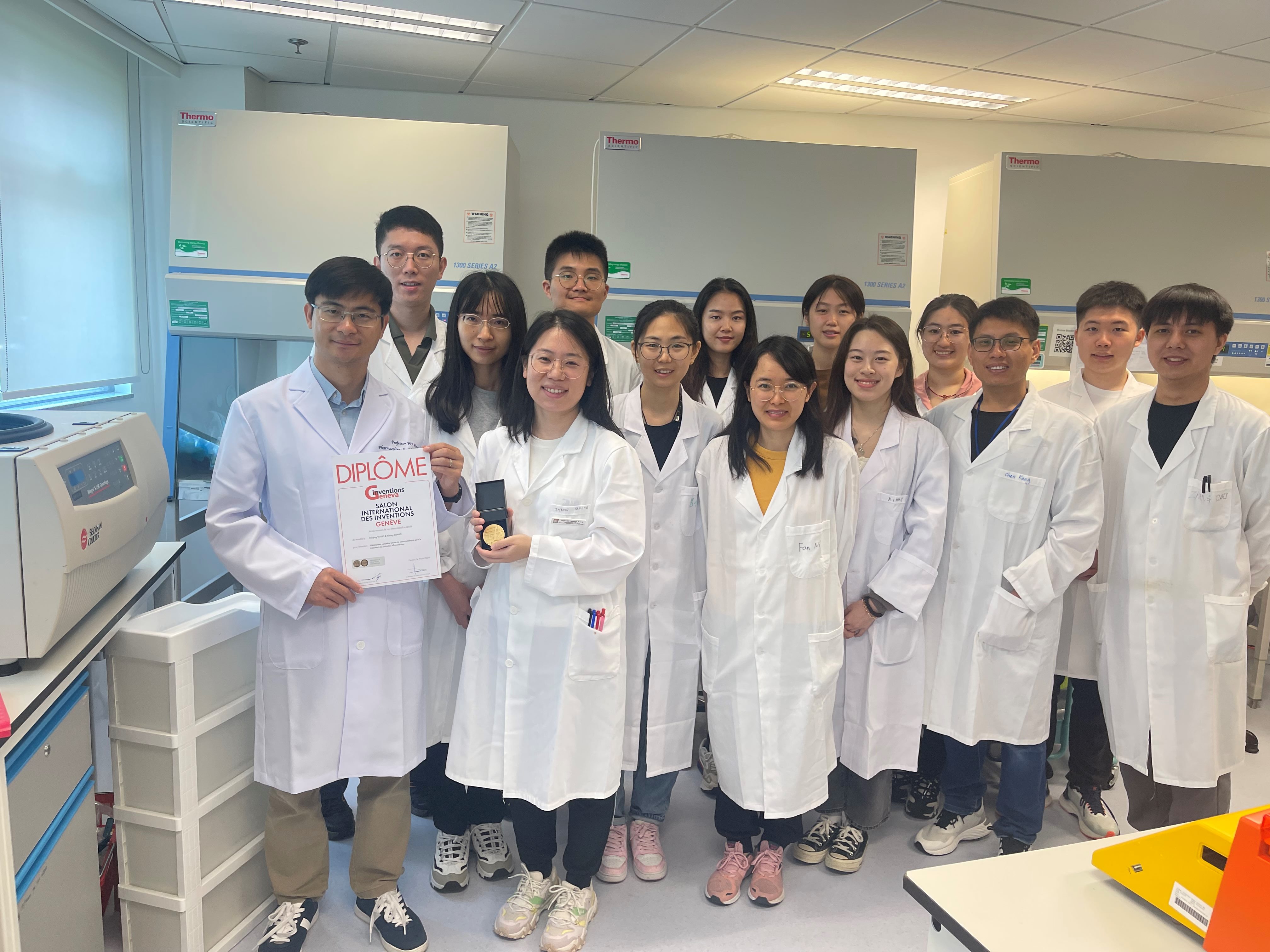
A cross-institutional research team led by the LKS Faculty of Medicine, the University of Hong Kong (HKUMed), has developed a novel cinnamaldehyde-based prodrug nanomedicine by utilising cinnamaldehyde, a common food additive, as an anti-inflammatory agent. The prodrug forms nanoparticles that deliver the therapeutic agents precisely to the inflamed sites, offering a solution for the treatment of inflammatory diseases like rheumatoid arthritis (RA). This innovative invention was awarded the 'Gold Medal' at the International Exhibition of Inventions of Geneva earlier this year. The research findings were published in Advanced Healthcare Materials [link to the publication], and a patent application was filed based on this work.
Background
Inflammation is a biological self-response mechanism to protect the human body from injury and infection caused by harmful stimuli. Generally, an inflammatory response can assist the body in self-defence and repair. However, dysregulated inflammatory responses may result in the development of various inflammatory diseases, such as RA and inflammatory bowel disease. The primary cause of these conditions involves the loosening of endothelial junctions, which allows inflammatory cell recruitment and infiltration into inflamed tissue. Subsequently, activated inflammatory cells promote the overproduction of various pro-inflammatory cytokines, which are responsible for the initiation and progression of inflammatory lesions. Therefore, the suppression of excessive pro-inflammatory cytokines is essential for the prevention, alleviation, and treatment of various inflammatory diseases.
RA is a common chronic inflammatory disorder caused by a dysregulated immune response, which affects 0.5-1% of the world's population. According to Hong Kong Arthritis & Rheumatism Foundation Limited, RA is a prevalent rheumatological disease in Hong Kong, and RA patients commonly experience various joint pains, continuous bone erosion and deformity throughout their bodies. As the disease progresses, the deterioration of the joints significantly impairs their ability to function, causing irreversible damage to their health and quality of life.
The current treatment strategies for inflammatory diseases involve primarily the use of anti-inflammatory medications, including non-steroidal anti-inflammatory drugs, steroids, and biological agents. In severe cases, surgical intervention may be required as an adjunct therapy. Despite remarkable advances in anti-inflammation and relief of clinical symptoms, the current treatment approach has been restricted by insufficient therapeutic efficacy and unfavourable systemic adverse effects due to the lack of targeting ability, poor stability, and low water solubility. Therefore, treating inflammatory diseases remains a significant challenge.
Research findings and significance
The research team has developed a new prodrug nanosystem using the FDA-approved food additive cinnamaldehyde to treat inflammatory diseases. Through chemical modification, the research team transformed cinnamaldehyde into a reactive oxygen species-responsive polymeric prodrug that can self-assemble into nanoparticles. In experiments on two mouse models with RA and ulcerative colitis, the researchers found that these nanoparticles effectively accumulated at inflamed sites of the mice through intravenous injection. The accumulated nanoparticles released cinnamaldehyde in response to high concentrations of reactive oxygen species at the inflamed sites, which alleviated the progression of inflammation by inhibiting the overproduction of pro-inflammatory cytokines. The results from the mouse model studies demonstrated that the cinnamaldehyde prodrug nanomedicine can be precisely delivered to the inflamed sites, unleashing their therapeutic effects without causing damage to other normal tissues.
Professor Wang Weiping, Associate Professor of Dr Li Dak-Sum Research Centre and Department of Pharmacology and Pharmacy, HKUMed, and the research member of the State Key Laboratory of Pharmaceutical Biotechnology, HKU, who led the research project, pointed out that this technology has three major benefits. ‘First, the team transformed cinnamaldehyde into a prodrug form through chemical modification, which can effectively improve the solubility and stability of the drug, making it easier for the body to absorb and maintain its activity,’ he explained. ‘Second, administering the drug in a nanoparticle form increases the accumulation of the drug at the site of inflammation, avoiding rapid metabolism of the drug and enhancing its therapeutic efficacy. Third, reactive oxygen species at the inflamed site can activate the drug to exert its effects in the affected area. The cinnamaldehyde prodrug has a better therapeutic efficacy than traditional drugs, providing a groundbreaking approach for targeted drug delivery in the treatment of inflammatory diseases.’
Professor Wang and his team are currently working on developing an oral dosage form of cinnamaldehyde prodrugs, to help patients easily comply with their doctor's instructions for medication and promote future clinical translation.
About the research team
The study was led by Professor Wang Weiping, Associate Professor of Dr Li Dak-Sum Research Centre and Department of Pharmacology and Pharmacy, HKUMed, and the research member of the State Key Laboratory of Pharmaceutical Biotechnology, HKU. The corresponding authors were Professor Guo Weisheng, School of Biomedical Engineering, Guangzhou Medical University, and Dr Li Zhongyu, College of Chemistry and Materials Engineering, Wenzhou University. The co-first authors were Dr Zhang Yaming and Dr Liu Lu, Postdoctoral fellows, Department of Pharmacology and Pharmacy, HKUMed. Other researchers included Dr Wang Tianyi, PhD graduate, Department of Pharmacology and Pharmacy, HKUMed; Mao Cong, master's student, School of Biomedical Engineering, Guangzhou Medical University; Shan Pengfei, Research Assistant, College of Chemistry and Materials Engineering, Wenzhou University; and Professor Chak-sing Lau, Dean of Medicine, HKU.
Acknowledgements
This work was supported by the Start-up Funds from HKU Dr Li Dak-Sum Research Centre and HKUMed, the National Natural Science Foundation of China, and the Natural Science Foundation of Guangdong Province of China.
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email (medmedia@hku.hk).

Follow HKUMed