01 April 2021
Mount Sinai researchers, in a collaboration with scientists at the LKS Faculty of Medicine, The University of Hong Kong (HKUMed), have found that a widely available and inexpensive drug targeting inflammatory genes has reduced morbidity and mortality in mice infected with SARS-CoV-2, the virus that causes COVID-19. In a study published in Cell (link to publication), the team reported that the drug, topotecan (TPT), a specific inhibitor of Topoisomerase I (TOP1), inhibited the expression of inflammatory genes in the lungs of mice as late as four days after infection, a finding with potential implications for treatment of humans.
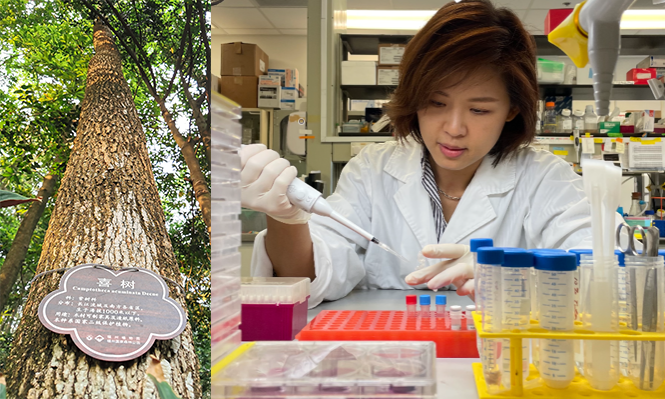
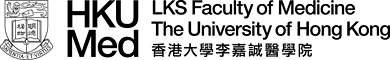
‘Topotecan (TPT) is derived from Camptothecin, a natural product that can be found in the bark of Chinese Happy tree. It is an inexpensive FDA-approved drug available in most countries around the world for use as anti-cancer agents,’ says co-lead author Bobo Mok, PhD, a scientific officer in the Department of Microbiology, HKUMed. ‘We demonstrated that TPT can also alleviate hyperinflammatory complications or cytokine storm of COVID-19 infection in hamsters,’ says Dr Mok.
The team’s research suggests that many other anti-inflammatory agents are less effective against COVID-19 because they target single inflammatory mediators, such as IL-6 or IL-1, or only specific gene expression programmes. ‘The fact is, a multitude of inflammatory genes and signaling pathways are dysregulated during a SARS-CoV-2 infection,’ explained another lead author Jessica Sook Yuin Ho, PhD, a postdoctoral researcher at the Icahn School of Medicine at Mount Sinai. ‘We demonstrated that TOP1 inhibitors were able to broadly dampen inflammatory gene expression in animal models, regardless of the gene or activation pathway.’
‘So far, in pre-clinical models of COVID-19, there are no therapies– either antiviral, antibody, or plasma – shown to improve SARS-CoV-2 infection outcomes when administered after more than one day post-infection,’ says senior author Ivan Marazzi, PhD, Associate Professor in the Microbiology Department at the Icahn School of Medicine. ‘This is a huge problem because people who have severe COVID-19 and get hospitalised, often do not present symptoms until many days after infection. We took a different approach, and sought to find a potential therapy that can be used during later stages of the disease. We found that TOP1 inhibitors given days after the infection can limit the expression of inflammatory genes in the lungs of infected animals to prevent an “hyper-inflammatory status”,’ says Dr Marazzi.
Although the pathophysiology of SARS-CoV-2 is not yet fully understood, scientists have observed that the virus triggers excess production of cytokines and chemokines – chemicals, which are secreted by cells of the immune system to help fight infection. An exaggerated immune system response, which characteristically occurs in the lungs of COVID-19 patients, can flood the infected area with white blood cells, resulting in inflammation, possible tissue damage, organ failure, and death. Reduction of the inflammatory state in such patients could therefore improve their clinical outcomes.
In a previous study published in Science in 2016, the same group at Mount Sinai found that inhibiting the activation of inflammatory genes could help prevent animal deaths from viral and bacterial infections, and suggested this could be a potent strategy against future pandemics. The current study – led by Mount Sinai along with partners from Singapore, Hong Kong, the United Kingdom, the United States and other global sites – expands on that earlier work to show how epigenetic therapy, which addresses the chemical modifications that influence gene expression, could be harnessed against severe cases of COVID-19.
The safety and efficacy of this treatment strategy in humans will soon be evaluated at clinical sites around the world, including India, where a trial recently began. The World Health Organization (WHO) is expected to play an important role in these studies.
HKUMed scientists who contributed to this research include Professor Chen Honglin, Professor of State Key Laboratory for Emerging Infectious Diseases and Department of Microbiology, Dr Honglian Liu, Post-doctoral Fellow, Ms Lau Siu-ying, Technical Manager, Dr Andrew Lee, Post-doctoral Fellow and Dr Anna Zhang, Scientific Officer, all from the Department of Microbiology.
About the Mount Sinai Health System
The Mount Sinai Health System is New York City's largest academic medical system, encompassing eight hospitals, a leading medical school, and a vast network of ambulatory practices throughout the greater New York region. Mount Sinai is a national and international source of unrivaled education, translational research and discovery, and collaborative clinical leadership ensuring that we deliver the highest quality care—from prevention to treatment of the most serious and complex human diseases. The Health System includes more than 7,200 physicians and features a robust and continually expanding network of multispecialty services.
About LKS Faculty of Medicine, The University of Hong Kong (HKUMed)
Founded as the Hong Kong College of Medicine for Chinese in 1887, the LKS Faculty of Medicine, The University of Hong Kong (HKUMed) became the premier founding Faculty when the University was established in 1911. From its modest beginnings, the Faculty has grown to become the largest faculty of the University. HKUMed is comprised of 14 departments and four schools with about 2,900 undergraduate and 1,700 postgraduate students. Teaching is conducted by more than 400 full-time teaching staff and about 3,000 honorary teachers, most of whom are doctors in public hospitals or private practitioners. For more information about HKUMed, please visit: www.med.hku.hk.
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email (medmedia@hku.hk).
Follow HKUMed